Clinical Pearls: Thromboelastography (TEG)
“There is no way you can possibly know how to interpret a TEG, I know anesthesiologists who do not understand them.” Should I tell you the story of that one time a very prideful physician said this to me? I’m not about the great healthcare profession divide. The one where we tear each other down because of a deep seated need to feed our egos. It comes from all sides docs to nurses, nurses to docs, etc. But I’ll tell you one thing, I’m for darn sure not going to let someone make me feel inferior. I already knew how to interpret and guide management based on TEG studies, but after this I made it a priority to deeply understand them.
The kicker of it all - TEG’s are REALLY not that hard to grasp. I know they seem confusing, but trust me, anything that has an algorithm is capable of making sense eventually. In this post I want to discuss my take on this study - what it measures and how it can guide management.
What is it?
A thromboelastogram is a study designed to tell you about hemostasis, in other words, when and how a clot is formed and then broken down (fibrinolysis). Traditionally this is measured by PT/PTT/INR which tell you extrinsic/intrinsic and common pathway problems that lead to bleeding or present a risk of bleeding. The TEG goes beyond this and offers you information about the aforementioned, plus platelet function, clot strength, and fibrinolysis. It is a study offered at many institutions and is most commonly utilized in the operating room or trauma settings. Increasingly, it is being seen more often utilized in emergency rooms and intensive care units. ROTEM is a slightly different test which gives you the same information but will not be covered in this discussion.
Who is it used for?
In the acutely bleeding patient you have to 1. stop the bleeding and 2. transfuse products and 3. reverse any coagulopathy. Several circumstances cause acute bleeding; trauma and surgery being the obvious offenders. I’d like to focus on the non-traumatic aka spontaneously bleeding patient. As you all know the acute gastrointestinal bleed patient can become an emergency case. If a coagulopathy is underlying or causing a patient to bleed it is critical that you reverse it in addition to numbers 1 and 2 mentioned previously. When someone has a serious coagulopathy, the blood is too thin and will not clot well. So you will be battling the body’s natural tendency to spontaneously bleed until you correct this. Therefore, it’s very important that you assess the patient’s ability to clot. You may see this type of bleed in:
acute or chronic liver failure
inherited bleeding disorders
someone on blood thinners particularly if they have or develop renal failure
anyone at risk of GI bleed, i.e. previous bleed, heavy NSAID use, ETOH use, esophageal varices, PUD, diverticular disease, etc.
hypothermia
thrombocytopenia
Leading to common locations of hemorrhage:
gastrointestinal system
intracerebral hemorrhage
retroperitoneum
surgical site
large joints
bladder
vaginal
less critical: epistaxis, oral mucosa or gingival, any insertion site
What does it tell me?
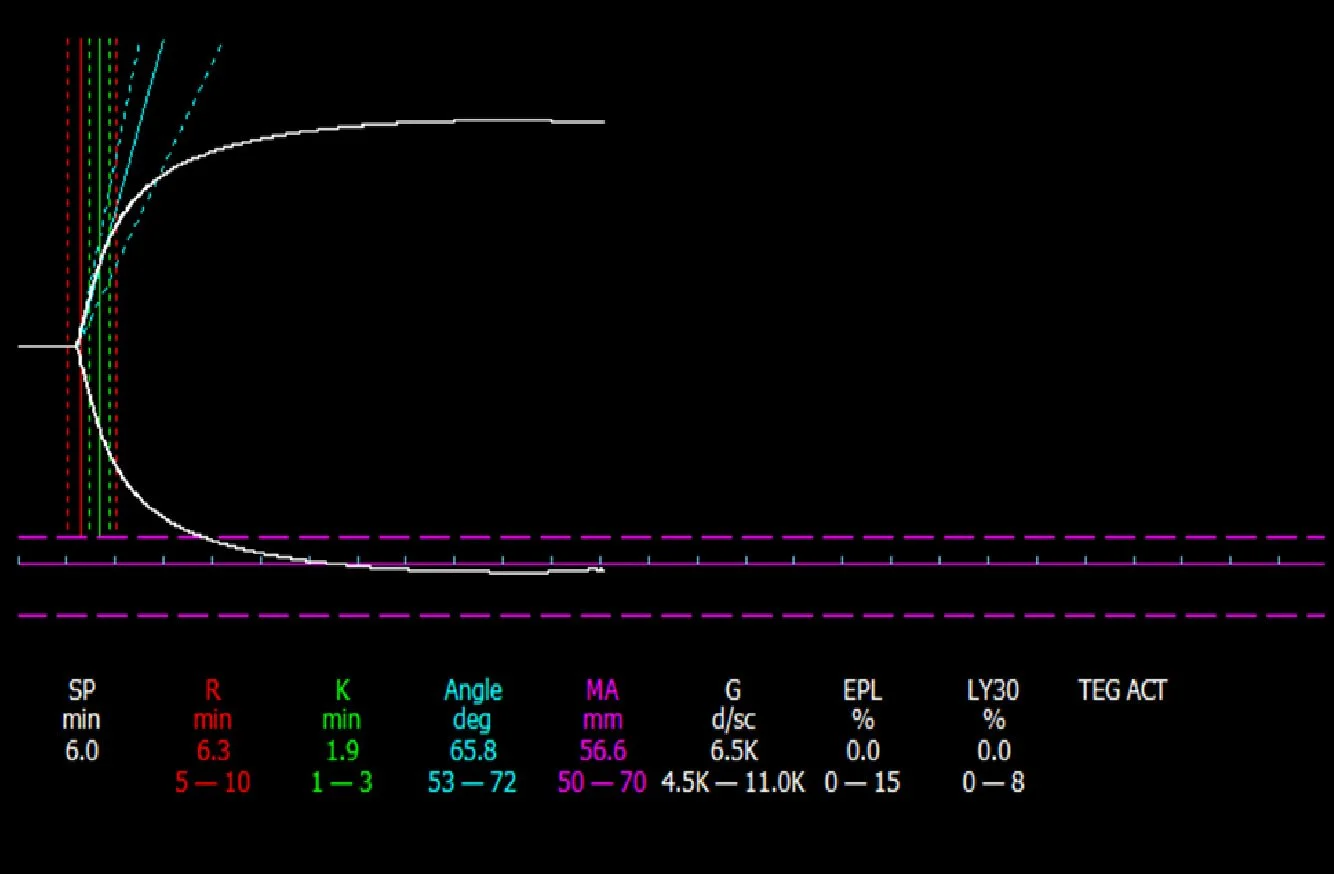
Remember the clotting cascade? (🤢) Do you recall the nine million steps to clot formation? I ask because appreciating the phases of thrombosis brings awareness to the many different phases in which it can fail. Pinpointing exactly where the coagulopathy lies helps you deliver the exact factor/product repletion needed. (You still need to give PRBC’s - anemia isn’t addressed by the TEG). The values you will assess are:
R time. This the time it takes for a clot to start forming. When it is too long you need to give FFP
K value. This is the period from the end of R until the clot reaches a certain angle. This is about speed of development. When this is prolonged give cryoprecipitate.
Alpha Angle. How quickly fibrin deposits build. When prolonged, give cryoprecipitate.
Maximum Amplitude. Measures height; strength. Looks at fibrin and platelet bonding. If low the wine glass will appear more like a champagne flute (thinner in the middle). Depending on severity give platelets or DDAVP.
LY30. the percentage of clot lysis after 30 minutes. This is measuring how much fibrinolysis is occurring. This one was the hardest for me to grasp. Think of it this way. We give clot busters (tPA) to break up clots. Too much tPA = big risk of bleeding. Why? Well you have induced fibrinolysis. This is the phase after a clot has formed when the body starts to break it down. If you have too much of this process you will continue to breakdown and therefore bleed (think tPA). So the antidote is Tranxemic Acid.
Click here to be redirected to RebelEM’s webpage where they discuss TEGs in cirrhotics. This graphic is from their site. I couldn’t make anything better than this easy/quick visual reference. Click here to be redirected to the IBCC’s very nice discussion on TEGs. Click here to be redirected to the Baylor approach which is what I use to guide treatment.
In the beginning I relied on the numerical values to interpret results, but as I’ve had more experience I can tell a lot from the visual as well. The TEG tracing is a wine glass. Normal should be a decent white wine with a short stem. Red wine and champagne are bad. No stem, while this is great in real life (less chance of toppling over) is not good on a TEG. An overly long stem is bad and reflects a prolonged R time (I find this and MA derangements to be the most common - perhaps anecdotal). Here are a few samples. First image: normal TEG. The last image: worst TEG I have ever seen. It represents late stage DIC. See if you can identify which values are poor and what you would give to manage.
Hope this helps and provides you with a useful new tool in managing your critical patient. And remember: adversity breeds strength. Use others’ insecurities as fuel to become better, not as fodder for your own insecurity.